Why do hemorrhoids bleed, and what are they?
Hemorrhoids, also known as piles, are dilated rectum and anus veins.
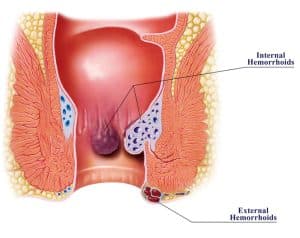
Hemorrhoids come in two varieties:
- Internal hemorrhoids: inside the rectum is where internal hemorrhoids grow.
- External hemorrhoids: external hemorrhoids form and grow under the skin, at the anal orifice.
Thrombosed hemorrhoids can develop from both internal and external hemorrhoids. Thrombosed hemorrhoids denote the formation of a blood clot within the vein. Thrombosed Hemorrhoids are normally not life-threatening, but they can be quite painful and inflamed. Rarely, is severe rectal bleeding from thrombosed hemorrhoids because of the surrounding skin’s ulceration (breaking) and necrosis (cell death). This demands urgent medical care.
For some individuals, hemorrhoids won’t show any symptoms to them. On the other hand, hemorrhoids can cause itchiness, stinging, bleeding, and discomfort, notably while you’re seated.
The surface of Hemorrhoids could be wounded by passing or straining a hard stool, which will make it bleed. All kinds of hemorrhoids can lead to bleeding. A thrombosed hemorrhoid may occasionally pop if it fills up too much.
What are bleeding internal hemorrhoids treatments at home?
A bleeding hemorrhoid is typically an indication that hemorrhoid’s surface has been irritated or injured. While this situation should eventually heal on its own, there are a few things you may do at home to hasten the process to reduce any discomfort.
We recommend visiting a colorectal specialist if the source of the bleeding is unclear or if it lasts longer than a week. Hemorrhoids are frequently self-diagnosed, which is risky, according to experts. Similar symptoms can be seen in a wide range of diseases, including cancer and IBD (inflammatory bowel disease). It’s crucial to get a precise diagnosis from a board-certified colorectal surgeon.
- Sitz bath. By submerging your anal part in a few inches of warm water. You can add some Epsom salts to the water to get even more relief.
- Wet wipes. External hemorrhoids may experience rubbing and irritation with toilet paper. Try using wet wipes to clean up instead. The wipes require no added scent or other allergens.
- Witch hazel wipe. Witch hazel pads or toilet paper are helpful to soothe and lessen irritation while cleaning up.
- Apply an ice pack. Sit on a cold pack wrapped in a towel to settle the area and minimize swelling. Apply for a maximum of 20 minutes at once.
- Avoid using the toilet for extended amounts of time or straining. This causes pressure on hemorrhoids and may worsen the situation.
- Make use of an OTC product. Medicated suppositories can be used for internal hemorrhoids and topical medications for external hemorrhoids. These treatments provide momentary relief with regular usage with the direction. Typically, you will feel better in about a week.
Medical treatment for bleeding internal hemorrhoids
Numerous surgical procedures can help with bleeding internal hemorrhoids if home remedies aren’t working. Many of the treatments don’t require general anesthesia and can be performed in the clinic.
- Rubber band ligation: Internal hemorrhoids can be confined with a rubber band by placing a little rubber band at its root. Due to the restriction of blood flow, the hemorrhoid eventually dries up and falls off after three to ten days.
- Sclerotherapy. This works similarly to rubber band ligation by injecting a medicinal treatment into a hemorrhoid. Usually, multiple injections are necessary, and the whole treatment lasts a few weeks
- Coagulation by using bipolar, laser, or infrared treatment. As a result, internal hemorrhoid loses its blood supply after one to two weeks, and eventually withers away.
- Electrocoagulation. An electrical current dries up the hemorrhoid, resulting in the formation of scar tissue and the eventual fall-off.
Also, make an effort to soften your stools, maintain a healthy digestive system and lower your chance of aggravating or damaging bleeding hemorrhoids more. Here is some advice:
- Hydration is key. To prevent constipation, drink sufficient amounts of water during the day.
- Consume fiber. Gradually increase your intake of foods containing high fiber such as whole grains, veggies, and fresh fruit. A high-fiber diet can avoid irregular stools and constipation.
- Constipation solution. Use an OTC suppository, hemorrhoid cream, or stool softener if you have constipation. However, follow up with your doctor if these don’t work after a week.
- Fiber supplement. If it’s hard to keep up with a high-fiber diet, you can also take a fiber supplement, such as methylcellulose or psyllium husk, which starts functioning within 1 to 3 days.
- Stay active. Constipation generally gets better with continued activity.
- Take polyethylene glycol (MiraLAX). It is safe for regular use. It results in a bowel movement within 1 to 3 days and draws water into your digestive tract to aid in softening the stool.
How to prevent hemorrhoids?
Lifestyle and diet adjustments are the key elements to preventing hemorrhoids. Here are five ways to avoid hemorrhoids in addition to maintaining a healthy weight, a balanced diet, and drinking lots of water.
- Personal hygiene. You can avoid hemorrhoids by maintaining a clean rectal area, especially after a bowel movement.
- Cotton underwear. Cotton fabric can keep the area dry to avoid bacteria.
- Avoid lifting heavy objects. The anal canal is put under excessive pressure when lifting heavy items.
- Do not sit for more than 15 minutes on the toilet. Using your phone or reading while on the toilet for an extended time puts strain on your rectum and anus.
When to see a doctor get rid of hemorrhoids?
If you notice blood, it’s advisable to see a colorectal doctor. While it might be hemorrhoid, it could also indicate more serious colorectal issues like colon cancer.
The first thing a doctor will probably do is check that the blood you’ve seen is coming from hemorrhoids. An experienced proctologist will perform palpation to check for internal hemorrhoids and external hemorrhoids. If the source of the blood is still unclear, they can advise a colonoscopy, which entails having a small, lit camera inserted into your colon while you’re unconscious. The doctor can look for any indications of additional conditions that might be the source of the bleeding.
Tell your colorectal specialist right away if you experience any of the following signs in addition to bleeding:
- Anal pain or changes in stool color or consistency
- bowel movements habits change
- abdomen pain, fever, and sudden weight loss
- light-headed
- dizziness or vomiting
Dr. Allen Kamrava is a board-certified proctologist and colorectal surgeon in Los Angeles. If you are experiencing any of the symptoms mentioned above, please book an appointment with Dr. Kamrava today!